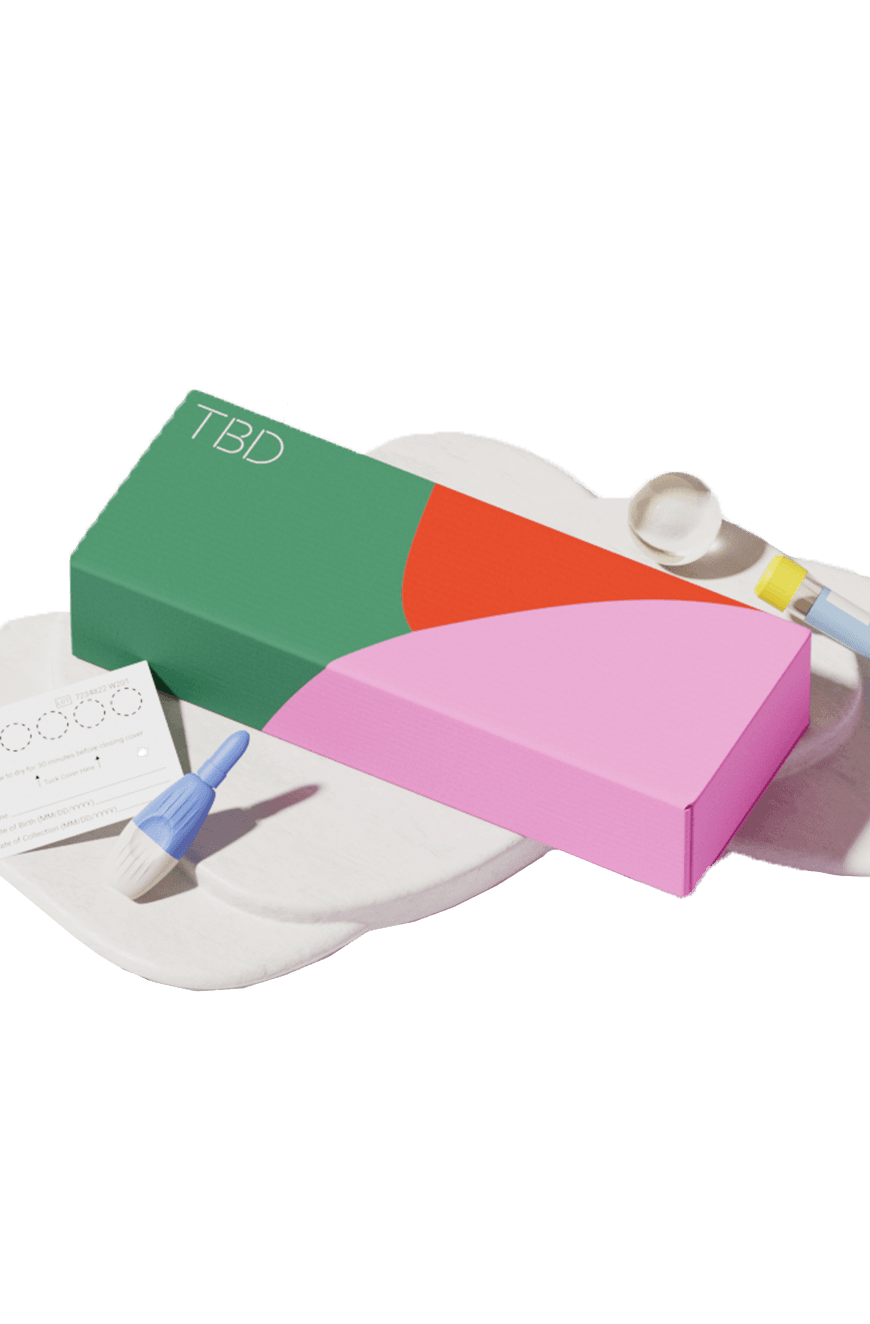
| TBD Panels | 3-Panel STD Test | 9-Panel STD Test | 5-Panel STD Test | 3 Site: Oral, Rectal, Genital |
|---|---|---|---|---|
| Chlamydia |  |  |  |  |
| Gonorrhea |  |  |  |  |
| Trichomoniasis |  |  |  | |
| HIV (Ag/Ab) |  |  | ||
| Syphilis |  |  | ||
| Hepatitis B & C |  | |||
| HSV I |  | |||
| HSV II |  |

- 8 E Charleston Blvd
- Las Vegas, NV 89104
- Tues and Fri
- 10 AM – 2PM
- Contact us:
- +1 (702) 909-0554
- hello@tbd.health

| TBD Panels | 3-Panel STD Test | 9-Panel STD Test | 5-Panel STD Test | 3 Site: Oral, Rectal, Genital |
|---|---|---|---|---|
| Chlamydia |  |  |  |  |
| Gonorrhea |  |  |  |  |
| Trichomoniasis |  |  |  | |
| HIV (Ag/Ab) |  |  | ||
| Syphilis |  |  | ||
| Hepatitis B & C |  | |||
| HSV I |  | |||
| HSV II |  |

Written By: Dr. Sophia Murphy, DBH, SXI
Healthcare providers are called upon to provide care and create safety for those they serve. Read on for a breakdown of different ways healthcare providers can be more gender affirming and inclusive towards the LGBTQIA+ community.
Disparities in Healthcare Access
Not all populations or groups of people have equal access to healthcare. As a minority group, LGBTQ+ individuals are often underserved, at rates that are significantly lower than their heterosexual counterparts (2). LGBTQ+ individuals often have less access to stable employment and health insurance as a consequence of discrimination; 25 states currently allow employers and businesses to deny services on the basis of gender identity and sexual orientation (1).
- When LGBTQ+ individuals do receive treatment, services often lack cultural competency and awareness. Even well-intended providers may have little to no exposure concerning LGBTQ+ culture, understanding around topics and language, or experience addressing concerns specific to the community. Ignorance can be a deterrent for LGBTQ+ individuals to even seek treatment as many report concerns that they will need to educate their providers in order to be treated holistically.
Read More: Disclosing Transgender Status to Intimate
Ways Healthcare Providers Can Be More Inclusive
Cultural Competency: If a provider is not familiar with or has had minimal interaction with the LGBTQ+ community, it’s imperative to seek out additional training! Any opportunity to learn more about the culture, the history, and the current challenges in the LGBTQ+ community can greatly enhance patient-provider rapport. It’s never an individual patient’s job to educate a provider about an entire community of people. Visit https://www.apa.org/topics/lgbtq/history for an introduction (5)!
Trauma-informed Practices: Being a member of any minority group is associated with higher rates of depression, anxiety, shame, and trauma. Having an approach to care that is trauma-informed creates a strong foundation for safety in care-delivery. The Substance Abuse Mental Health Services Administration (SAMSHA)(4) states the following regarding trauma-informed care: Trauma-informed approaches to care shift the focus from “What’s wrong with you?” to “What happened to you?” by:
- Realizing the widespread impact of trauma and understanding potential paths for recovery 2.Recognizing the signs and symptoms of trauma in individual clients, families, and staff
- Integrating knowledge about trauma into policies, procedures, and practices
- Seeking to actively resist re-traumatization (i.e., avoid creating an environment that inadvertently reminds patients of their traumatic experiences and causes them to experience emotional and biological stress).
In addition to seeking out and completing continuing education in LGBTQ+ cultural competencies, providers have a responsibility to ensure they are aware of and proficient in trauma-informed practices. Be mindful and stay aware of your intentions to prevent actions from becoming performative (1).
Terminology: The nuances of language have the power to connect or drive disconnection. While it’s important not to create unrealistic expectations of perfectionism or “police” the language of others, providers can increase their ability to build rapport by being intentional and mindful in the language they use. When all else fails, ask! It’s more helpful to admit a knowledge gap, address a mistake, or ask for clarification, than it is to avoid feeling uncomfortable in a provider-patient interaction. Understand the importance of respecting someone’s pronouns and never assume someone’s gender identity based on their biological sex or perceived gender. The same is true for family structures. Avoid assuming someone’s relationship status, the gender or pronouns for a partner, or even the idea that someone has only one partner! Increase your ability to ask open-ended questions and use gender-neutral language when available. See some examples below:
- “Hi! My name is Dr. Murphy and my pronouns are she/her, what would you like me to call you and what are your pronouns?”
- “What do you call your body parts?” (For use in medical settings where you may need to examine a patient’s body)
- “Who comprises your family?”
- “Who is your support system?”
- “How do you describe your family?”
- “What does sexual activity look like for you?” (For settings focused on sexual health and wellness)
- Visit https://www.genderbread.org/resource/genderbread-person-minimal-3-3 for helpful resources on understanding the differences between sex, gender, gender identity, sexual orientation, romantic affiliation, and other terminology support (3)!
Learn More: Celebrating PRIDE Month by Celebrating Yourself!
All People Deserve Safe and Effective Healthcare
Being a member of a minority group is associated with poorer health outcomes overall in comparison to dominant culture groups. Heart health for LGBTQ+ individuals is often poor as a complication from living with increased stress associated with social discrimination (1). When a patient experiences rejection, discrimination, or a general lack of understanding around nuances of their identity(ies), it’s harder to build trust with medical providers. In recent years, states have begun banning medical care for gender-affirming treatment, essentially denying the existence of an entire group within the LGBTQ+ community (1).
Poor past interactions or a general mistrust of medical providers overall often deters LGBTQ+ patients from seeking treatment, especially preventative care. All people deserve access to healthcare and all people deserve to receive healthcare free from discrimination. For a patient to feel safe, to be honest, and to feel secure in accepting medical intervention, an environment of acceptance and curiosity goes a long way. As providers who commit to providing exceptional care, we owe it to ourselves as practitioners, and our patients and community as a whole, to ensure we close knowledge gaps, explore unconscious biases, and challenge what we find (implicit and explicit). When any group suffers, the collective suffers. By creating opportunities for safe and effective healthcare (specifically for our most underserved groups), we create change that ripples everywhere.
References:
- BetterUp. (2022, May 20). LGBTQ health disparities: Finding better care, safety, and well-being. https://www.betterup.com/blog/lgbtq-health-disparities
- Cigna Healthcare. (n.d). LGBTQ+ Health disparities. https://www.cigna.com/knowledge-center/lgbt-disparities#:~:text=LGBTQ%2B%20people%20are%20less%20likely%20to%20have%20a%20regular%20health%20care%20provider.&text=Lesbian%20and%20bisexual%20women%20have,women%20are%20at%20greater%20risk.&text=LGBTQ%2B%20people%20have%20higher%20rates,related%20cervical%20or%20anal%20cancers.
- The Genderbread Person. (n.d). https://www.genderbread.org/
- Menschner, C. & Maul, A. (2016). Key ingredients for successful trauma-informed care implementation. https://www.samhsa.gov/sites/default/files/programscampaigns/childrensmental_health/atc-whitepaper-040616.pdf
- Morris, B.J. (2023). A brief history of lesbian, gay, bisexual, and transgender social movements. https://www.apa.org/topics/lgbtq/history
This article provides information about sexual health, healthcare and/or related subjects. The blog content and any linked materials herein are not intended to be, and should not be construed as a substitute for, medical or healthcare advice, diagnosis or treatment. Any reader or person with a medical concern should consult with an appropriately-licensed physician or other healthcare provider. This blog is provided purely for informational purposes. The views expressed herein are not sponsored by and do not represent the opinions of TBD Health Inc.



Email us and a team member will get back to you within 24 hours. We’re also available via call or text at +1 (702) 909-0554
Sign up below to get 10% off
By providing my email address, I agree to receive email with marketing communications from TBD Health including news, promotions and exclusive offers. I understand that I can opt out at any time by using unsubscribe links. Visit our Terms of Service or Privacy Policy for more information.